Help designing, developing, implementing, and/or operating:
Innovative Crisis Response Services & Systems-Level Improvements
We Offer
Crisis Response Services
- Crisis Stabilization Centers
- Rose Houses: Peer-Operated Crisis Respites
- Forensic Mobile Crisis & Response Teams
- Peer Services in Hospital or Clinic Settings
- Transitional Care Wellness Teams
Systems-Level Improvements
- Integration: Whole Community Systems Transformation
- Training: Behavioral Health Workforce and Culture
Interested In Learning More?
Contact us at [email protected]
Who We Are
People USA is a peer-run behavioral health organization that creates, provides, and promotes innovative crisis response services and systems-level improvements throughout the United States and the world.
We have spent over three decades designing, developing, implementing, and operating services and systems that effectively address the enormous challenges that we face.
We bring our expertise to you, so that you too can:
- Reduce hospital emergency room visits, inpatient admissions, & readmissions.
- Reduce incarceration due to under-addressed behavioral health issues.
- Achieve the Triple Aim: (i) Improved care delivery & customer satisfaction, (ii) Better health outcomes, (iii) Reduced public costs
- Create an effective system of care that works better for your community.
We Are Facing Unprecedented Challenges
De-Institutionalization.
Our nation shifted large populations away from long-term care facilities, like state-run psychiatric centers, without ensuring that people had the skills, supports, and resources they need to thrive in community.
Opioid Epidemic.
We are in the midst of a national public health crisis, made worse than ever by synthetic opioids, with alarming and increasing rates of addiction, overdoses, and deaths.
Social Determinants of Health.
Social isolation, economic stress, and housing instability are causing and worsening population health outcomes, including mental health, addiction, and chronic physical health issues like heart disease, respiratory illness, and diabetes.
Trauma.
Research continues to show trauma’s universal reach and its lasting adverse effects – emotional, physical, cognitive, behavioral, and existential – which can be felt for years, decades, whole lives, and even generations to come.
Suicide.
The other national public health epidemic, suicide continues to be a top-10 leading cause of death in the U.S., and the suicide death rate – now more than two times greater than homicides – continues to rise year-to-year.
Chronic Underfunding.
Mental health and addiction services have never been funded adequately, they are constantly at risk of deep cuts, and service providers consistently have to do more with less.
Traditional Responses Have Generally Not Worked
Hospitals.
Hospital emergency behavioral health services are utilized far beyond capacity, driving public costs up to unsustainable levels. Hospitals are also struggling to provide the type of quality care that people need and want during and after a behavioral health crisis. The overall system is not preventing avoidable ER visits, inpatient admissions, and readmissions.
Jails.
Jails have become our nation’s largest mental health and addiction treatment centers, which are inhumane, ineffective, and also very costly places to provide care.
Community-Based Service Providers.
Community-based health, human, and social service providers, the frontlines in prevention, lack adequate coordination, making the entire system difficult to navigate, and impossible for people to get their whole health needs met at once.
Overall System Culture.
Our whole system of care is still struggling to operate in line with core values, behaviors, and best practices that actually facilitate recovery and wellness.
The Triple Aim.
And it has seemed nearly impossible to achieve the important, simultaneous goals of the Triple Aim: (i) Improved care delivery & customer satisfaction, (ii) Better health outcomes, and (iii) Reduced costs.
People USA’s Solutions Do
Crisis Stabilization Centers can help you to significantly reduce hospital utilization and incarceration rates, improve your local crisis response services and coordination, and create a more welcoming gateway to your local health, human, and social services system.
Rose Houses (Peer-operated Crisis Respites) can help you to reduce hospital ER visits, inpatient admissions, and readmissions; and provide your community with superior emergency mental health services that are engaging, trauma-informed, empathetic, hopeful, and proven to produce better health & quality of life outcomes.
Forensic Mobile Crisis & Response Teams can help you to reduce incarceration rates, improve your police responses and court treatment options, and ensure that people presenting with behavioral health issues receive immediate care and connections to services, so that they can stay out of the criminal justice system whenever appropriate and possible.
Integrated Peer Services (in Hospitals or Clinics) can help you add value to your “traditional” emergency, inpatient, or outpatient operations by reducing lengths of stay; and improving patient engagement, patient activation, care delivery & customer satisfaction, treatment planning, and discharge plan effectiveness.
Transitional Care Wellness Teams can help you to reduce hospital ER visits, inpatient admissions, and readmissions; provide people with more hands-on education, support, and empowerment to ensure their discharge plans actually work; improve continuity of care by bridging the gap between the hospital and community-based service providers; and improve people’s health & wellness literacy, self-management skills, and outcomes.
Integration: Whole Community Systems Transformation can help you to reduce hospital utilization and incarceration rates, improve population health outcomes, reduce public costs through improved efficiencies, and raise the bar for your local system of care on accessibility, customer engagement, collaboration & teamwork, whole health oversight, person-centered care, and “no wrong door” approaches – breaking down obsolete silos.
Training: Behavioral Health Workforce and Culture can help you to improve service delivery, effectiveness, efficiency, and value; and ultimately raise the bar in high-impact areas, including but not limited to: High-Quality Customer Service; Person-Centered Engagement; Trauma-Responsive Care; Empathy and Mutuality; Recovery Culture; Whole Health / Wellness Outcomes.
Dramatic Cost Savings
- Each Crisis Stabilization Center can serve up to 5,480 people annually, and saves the system over $12.28 million per year.
- Each Rose House can serve up to 500 people annually, and saves the system over $6.57 million per year.
- Each Forensic Mobile Crisis & Response Team can serve up to 300 people annually, and saves the system over $5 million per year.
- Each Peer Integrated into a Hospital can serve up to 500 people annually, and saves the system over $1.3 million per year.
- Each Transitional Care Wellness Team can serve up to 300 people annually, and saves the system over $3.75 million per year.
Total Savings: over $28.93 million per year.
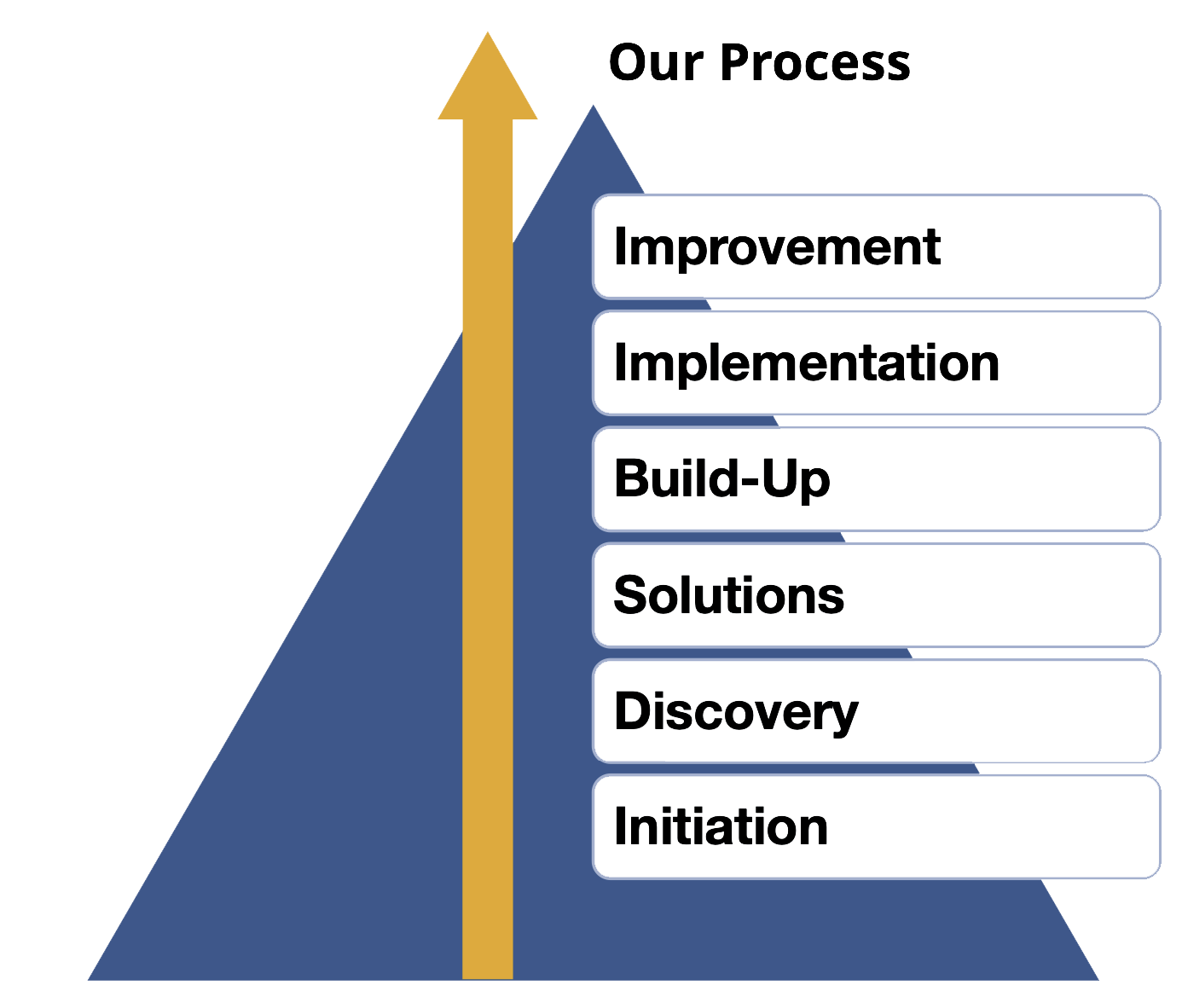
Where We Begin
We first work with our clients to determine their needs , and how we can best assist them. This involves exploring core areas:
Needs: Fully framing the issue or opportunity to be addressed, its impact, and any relevant research.
Objectives: Clearly setting goals or objectives that flow logically from identified needs.
Procedures: A detailed action plan outlining how objectives will be met.
Personnel: Identifying all staff needed to actualize the work, what they will do, and their various qualifications, skills, and experiences.
Support: Identifying various stakeholders who will need to be engaged with to ensure success.
Evaluation: Determining the means and methods by which each objective will be tracked, and how results will be reported to stakeholders.
Budget: A comprehensive budget and narrative outlining and justifying all costs needed to implement the roadmap.
People USA’s Résumé
Crisis Stabilization Centers
People USA worked with Dutchess County Government (NY), and a Broad Coalition of Community Service Providers, to create the Dutchess County Stabilization Center, the Northeast’s first crisis stabilization center, in Poughkeepsie, NY.
Rose Houses: Peer-run Crisis Respites
People USA has helped nonprofit organizations and local government units to open 39 Peer-operated Crisis Respites in Alaska, California, Georgia, Massachusetts, Michigan, Minnesota, Nebraska, New Jersey, New York, North Carolina, Pennsylvania, Vermont, Washington, Wisconsin, and Europe – multiple in Netherlands.
Forensic Mobile Crisis & Response Teams
People USA worked with Westchester County Department of Community Mental Health (NY) to create the Westchester Crisis Stabilization Team, the first peer-run criminal justice-focused mobile team in the United States.
Peer Services: Hospital or Clinic Settings
People USA has helped hospitals like Kings County Hospital (NY), HealthAlliance Hospital (NY), and MidHudson Regional Hospital (NY); and clinical providers like New York City Department of Health and Mental Hygiene, and Mental Health Association (MHA) of Nebraska to infuse peer services into their clinical operations.
Transitional Care Wellness Teams
People USA has helped Westchester Medical Center Health Network, and Adirondack Health Institute—two organizations working with New York State to achieve major reductions in avoidable hospital use and Medicaid spending—to create transitional care programs.
Integration: Systems Transformation
We have successfully engaged in Community-Wide System Transformation in Dutchess County, NY, Ulster County, NY, and Orange County, NY.
Training: BH Workforce & Culture
We have successfully helped Kings County Hospital (NY); North Carolina Division of Mental Health, Developmental Disabilities and Substance Abuse Services; New York City Department of Health and Mental Hygiene; and Mental Health Association (MHA) of Nebraska to enhance their workforces and overall cultures.

